Fibromyalgia: Is it real life or is it just fantasy?
- UoG Journalism Students

- Dec 13, 2018
- 5 min read
Updated: Dec 14, 2018
Have you ever had the infuriating misfortune of stubbing your toe? Try to remember the pain you experienced in that moment, then reminisce in the calmness that comes afterwards. Now, imagine experiencing that same pain for an hour when you wake up in the morning – it sounds awful, right?
Most times, pain functions primarily as an alarm, working to interrupt all other concerns, goals, desires and motivations, and impose a new priority of escaping pain or its causes. For most people and in most situations, pain is only temporary. That’s not the case for many individuals, their pain proves to be long-lasting and life changing.
Pain can be the one factor that stands in the way of achieving dreams or simply getting out of bed. Many people around the globe suffer from an invisible illness that comes with a wholly destructive experience. That illness has many names and countless symptoms, but the product is always the same, a crippling chronic pain.
What’s the fuss about? Surely there is a medicine or a drug that could help? The answer is simply: no.
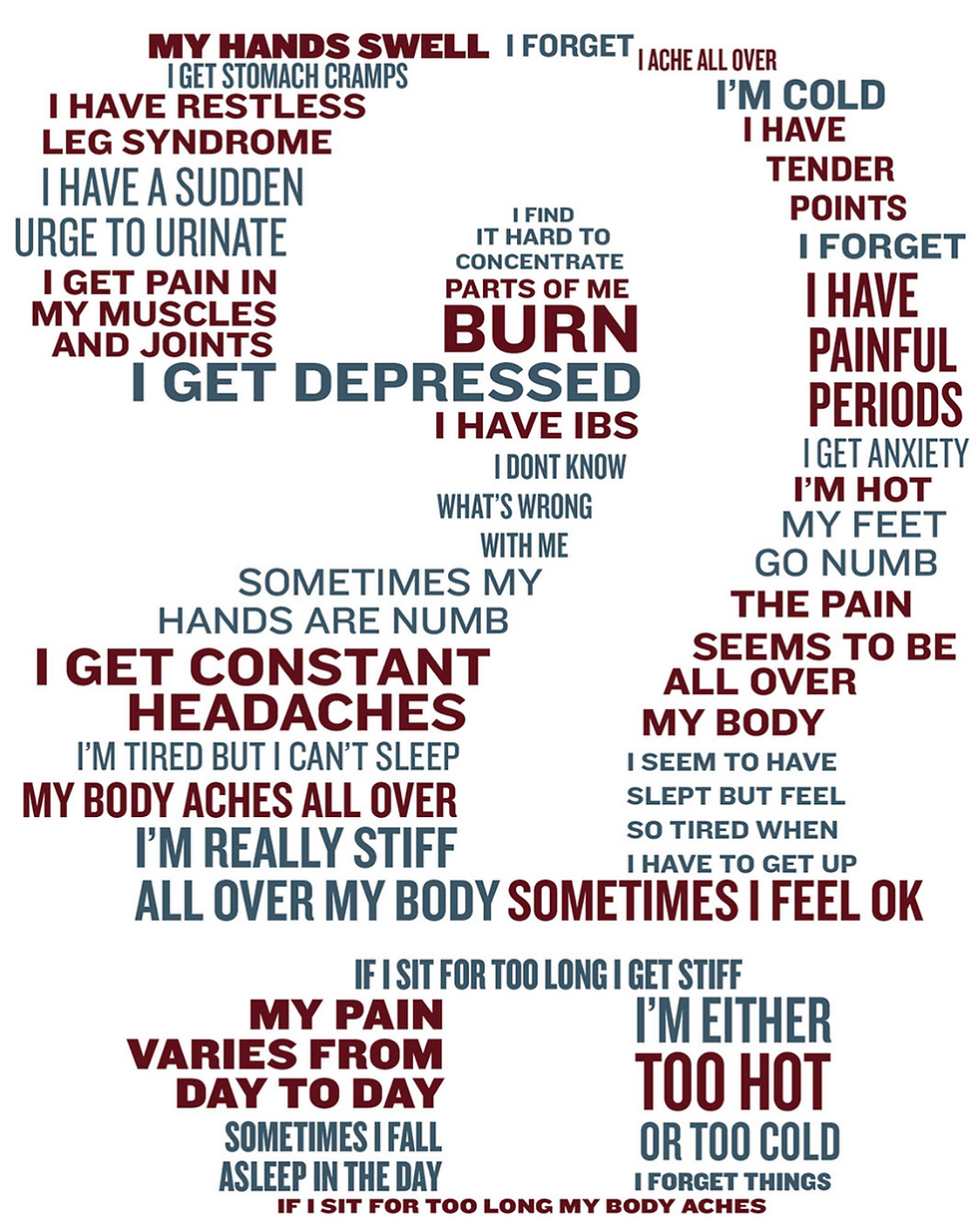
That illness is fibromyalgia. Currently, there isn’t a text book answer as to what fibromyalgia is and there is no cure - it’s called the invisible illness for a reason. Most people with fibromyalgia suffer for months and, in some cases, years until they get a diagnosis because nothing shows up on tests or scans. It is often a last-ditch diagnosis once everything else is ruled out. It has also been an ongoing debate about whether patients scapegoat the illness itself. This raised the question, is fibromyalgia real or has a stigma made us believe it’s not?
Failing to find much scientific evidence to answer that question, understanding the patients’ experiences is vital. There are individuals who live with it, hate it, and who are frustrated by the stigma behind it.

To achieve her dream of landing a role on the West End, Urdang musical theatre student, Vanessa has to work extra hard to take care of her body, and she uses the art of dance to numb the pain. She was diagnosed with fibromyalgia in May 2018. She also created her own routine with doctors and physiotherapists, in order to deal with the pain, using body
conditioning exercises and a cocktail of painkillers. Vanessa is very outspoken about the stigma behind fibromyalgia as it’s being dismissed as a fake illness, and some people still refer to it as the ‘yuppie flu.’
“My journey was a little non-traditional. I got a migraine that lasted for five weeks. It went away for a while. Then, three months later, the migraine came back. This time it lasted for nine months. I was up to my ears in medical tests. I was in such an exaggerated state of pain that one day, in addition to the migraine, I just couldn’t move. The pain had just spread everywhere. That was what instigated my fibromyalgia diagnosis. The way my doctors explained it, the trauma of the migraine kind of freaked my body out to the point where I then developed fibromyalgia.”

The time frame of Vanessa’s diagnosis isn’t rare, it’s actually the norm. A study conducted by the Fibromyalgia Association in the UK (FMAUK), shows that most sufferers have to go through a minimum of eight different tests, and with the ever-growing pressures on the NHS, those eight tests can take up to a year to be completed due to the waiting lists. Despite the NHS’ simple worded fibromyalgia diagnosis criteria, which states:
“If you have a widespread pain index (WPI) score of seven or higher and you’ve experienced symptoms at a similar level for at least three months.”

Vanessa scored a crippling twelve on the WPI, yet she said “I was very optimistic throughout the whole process. I remember one time, I was getting some results back at the hospital. I was so shocked from the results, that I actually triggered a pain episode and started crying. I just sucked it up and asked the same question, I always ask: 'what now?'”
Unfortunately, she is not alone. According to FMAUK, an estimate of 1.5 – 2 million people suffer with the chronic illness. Many people don’t even seek medical help as they are unaware of the illness and its symptoms, or they are misdiagnosed by GPs.
Dr Janet Horton from the British Psychological Society, says: “The medical community knows so little about the illness, so it’s a lot of trial and error. There are medicines you can take, but they can be very hit or miss. A lot of chronic illness patients use and rely on painkillers and opiates to get through the day. It’s a physical illness with physical symptoms, but it’s perpetrated by psychological traumas.”
When asked about how she feels about the stigma of it being a ‘fake illness’ – her response was nothing short of profound.
Dr Horton says: “It’s quite scary that academics and some people, who have had very advanced training and education – share that ignorant view. Fibromyalgia goes beyond opinions or theory, it’s science. It’s black and white. It affects over a million people in this country alone and an estimate of 400 million people around the globe.”

On the other hand, Dr George Ehrlich publisher of “The Journal of Rheumatology” says: “When one has tuberculosis, one has tuberculosis, whether or not it is diagnosed. The same is true for cancer, rheumatoid arthritis and hookworm infestation. However, FM is purely psychological. it’s all in the patient’s head and it needs to be treated as a mental illness… some hypochondriacs use a FM as an excuse to skip work – that is wrong.”
When Vanessa read Dr Ehrlich’s comment on the matter, she teared up and simply replied: “This has been my struggle for the past couple of years. I am not even shocked, I am just sad and sorry for myself. I am a 22-year-old woman, with a dream to perform and the pain of people denying my struggle hurts more than the actual physical pain.”

Fibromyalgia presents as a cluster of nebulous symptoms, and there is no definitive cure, so treatments are based on trial and error. This can be tremendously frustrating to physicians and that means patients suffer.
"Sometimes (doctors) take out their frustrations on the patients and blame the patients for the illnesses," says fibromyalgia expert Daniel Clauw, MD, director of the Chronic Pain and Fatigue Research Centre at the University of Michigan. "There's a long history of this in medicine."
This is inexcusable in 2018, Patrick Wood, MD, a senior medical adviser to the National Fibromyalgia Association, believes that sexism may be at the root of this.
"Why in this society are we so free to dismiss the complaints of 20- to 50-year-old women? Why can we marginalize their experience so easily? It really does become an issue of gender politics. Why can we marginalize her and disregard her complaint, and yet if she were a man the same age we might take her seriously?"
Scepticism extends beyond the medical community. It can be difficult claiming a medical condition in everyday life when, on the outside at least, you appear fine or you act fine.
After Vanessa calmed herself, she expressed a day-to-day problem she experiences that perfectly sums up the stigma.

So, if you are a doctor or someone who would question a person parking in a disabled spot, just remember the pain you go through when you stub your toe. Then, instead of judging or coming up with your own notion, be empathetic and offer support cause you never know what this person is going through. For someone like Vanessa, the pain stands between her and her dreams of being on stage.








Comments